







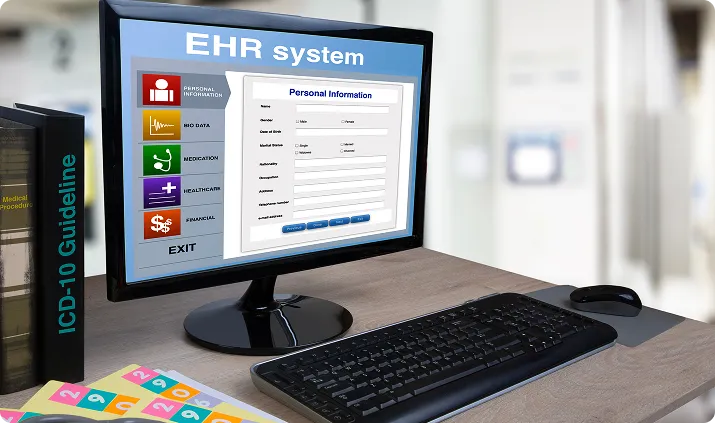
We integrate directly with leading EHRs to pull encounter data, diagnoses, and charges into the claims engine, enabling real-time claim generation and submission.

Our platform connects with major clearinghouses to support 837 claims, 835 ERAs, and 270/271 eligibility checks, ensuring clean submission and fast response cycles.

We offer direct API integration with top payers to enable claim status checks (276/277), real-time adjudication updates, and payment tracking.

Sync medical billing software’s claim data, payments, and remittances with your Practice Management software to unify financial reporting and streamline denial workflows.

Team Folio3 brought my dream app to reality, they explained every step to our non technical team professionally. wireframe and design processes were outstanding & they built stunning and perfectly integrated application. I think both patients and clinic will be significantly benefited.





Working with the folio3 team has been a great experience. Your dedication, creativity, and adaptability in overcoming challenges for the Moodology app project are truly commendable.


I appreciate your remarkable work during the recent Laboratory service phase. Your determination, analytical thinking, and continuous efforts were crucial in overcoming challenges and achieving success. I appreciate your help as we collaborate to create fantastic items.

Kudos to your team for outstanding work in the discovery phase! Your team understood our business and workflows by asking the right questions and extracting the most useful information. Your team's ownership and results-oriented approach are commendable.