






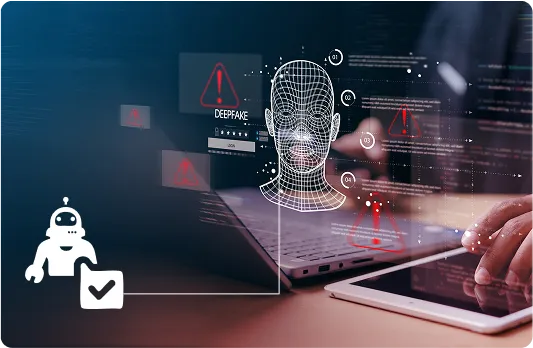


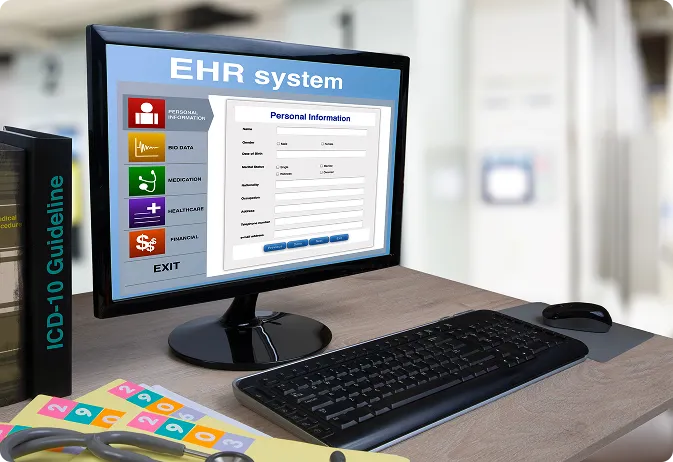
Connects with patient records to surface billing-service mismatches using clinical context. Built to offer EHR and specifically Epic Integration.

Works across your existing medical billing software and claims infrastructure, detecting fraud pre-payment without delaying adjudication or reimbursements.

Feeds real-time logs into your audit systems, supporting HIPAA-compliant software and CMS requirements with zero manual overhead.
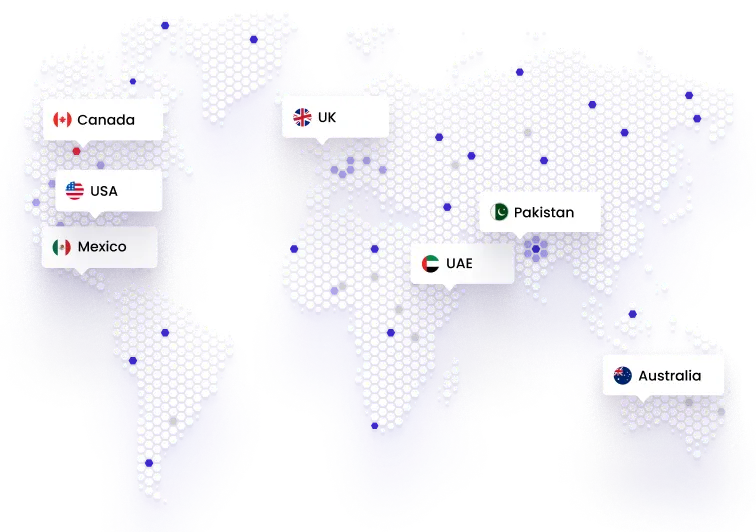
With decades of experience in healthcare and digital health, we understand the nuances of the industry and tailor solutions that perfectly align with your specifications and fit your workflow.
Our solutions are sophisticatedly designed to not only meet your requirements but also to keep you audit-ready by ensuring they adhere to industry and regulatory requirements like HIPAA, GDPR, and others.
From initial discovery to implementation and beyond, our team provides complete support ot ensure that your operations remain uninterrupted while they adapt to the innovative shift.

Team Folio3 brought my dream app to reality, they explained every step to our non technical team professionally. wireframe and design processes were outstanding & they built stunning and perfectly integrated application. I think both patients and clinic will be significantly benefited.





Working with the folio3 team has been a great experience. Your dedication, creativity, and adaptability in overcoming challenges for the Moodology app project are truly commendable.


I appreciate your remarkable work during the recent Laboratory service phase. Your determination, analytical thinking, and continuous efforts were crucial in overcoming challenges and achieving success. I appreciate your help as we collaborate to create fantastic items.

Kudos to your team for outstanding work in the discovery phase! Your team understood our business and workflows by asking the right questions and extracting the most useful information. Your team's ownership and results-oriented approach are commendable.